Rehabs for Physical/Sexual Abuse

Showing 20 of 37 Results (filtered)
Featured Rehab Centers



Addiction Rehab Centers - ARC At Bayside | Indianapolis Drug & Alcohol Rehab
Indianapolis, Indiana
5929 Lakeside Blvd, Indianapolis, IN 46278




Hamilton Center Inc: Mathew Maleakal S MD
Terre Haute, Indiana
620 8th Ave, Terre Haute, IN 47804
Get Personalized Rehab Matches in 60 Seconds
Tell us a few details and we’ll show a personalized shortlist of verified Indiana rehabs, making it simple to compare options and choose your next step with confidence.



Indiana Center for Recovery - Alcohol & Drug Rehab Center Jeffersonville
Jeffersonville, Indiana
601 N Shore Dr Suite 102-103, Jeffersonville, IN 47130



New Vista North
Indianapolis, Indiana
4010 W 86th St suite d, Indianapolis, IN 46268



Boca Recovery Center - Fort Wayne, Indiana
Fort Wayne, Indiana
111 W Berry St #211, Fort Wayne, IN 46802
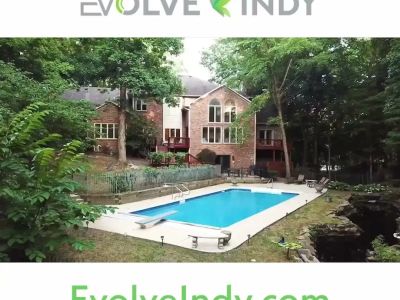


Evolve Indy
Indianapolis, Indiana
8770 Guion Rd, Indianapolis, IN, 46268



See Purpose Addiction Treatment Center Indiana
Bloomfield, Indiana
3237 IN-157, Bloomfield, IN 47424



Boca Recovery Center - Indiana Drug and Alcohol Rehab
Huntington, Indiana
3040 W Park Dr, Huntington, IN 46750



First City Recovery Center
Kokomo, Indiana
317 W Jefferson St, Kokomo, IN, 46901



Parkdale Center
Chesterton, Indiana
350 Indian Boundary Rd., Chesterton, IN, 46304

Centerstone - North Bevcher Drive
Madison, Indiana
3008 North Bevcher Drive, Madison, IN, 47250


Centerstone Recovery Center
Richmond, Indiana
1811 S 9th St, Richmond, IN 47374



Aspire Indiana Health - Hoak
Anderson, Indiana
2009 Brown Street, Anderson, IN, 46016



Caring About People - Counseling
Fort Wayne, Indiana
1417 N Anthony Blvd, Fort Wayne, IN 46805



Pinnacle Treatment Centers - Cambridge City
Cambridge City, Indiana
2060 State Road 1 North, Cambridge City, IN, 47327



YWCA of North Central Indiana
South Bend, Indiana
1102 South Fellows Street, South Bend, IN 46601

Center for Positive Change
South Bend, Indiana
611 Lincolnway East, South Bend, IN 46601



Dove Recovery House for Women
Indianapolis, Indiana
3351 N Meridian St #110, Indianapolis, IN 46208



Eskenazi Health - Sandra Eskenazi Mental Health Center - N. Meridian St
Indianapolis, Indiana
3171 N. Meridian St., Indianapolis, IN, 46208
Why Trust Indiana Rehabs
As Hoosiers helping Hoosiers, we understand the unique challenges our communities face. Our team meticulously verifies every Indiana treatment center, ensuring you find trusted, local care that truly understands your journey.
About our listingsLevels of Care
Explore popular treatment options by levels of care, from flexible treatment in Outpatient centers to intensive care in Residential rehabs.
Free · 24/7 · Confidential
Talk to a Treatment Specialist
Call now to get matched with Indiana facilities that accept your insurance.
(888) 568-9930
Free
Ins. check
4.9★
Rating
HIPAA
Protected
Can't travel to a facility?
Licensed Indiana therapists via secure video — same-week appointments, evenings & weekends available.
Just reaching out for information after physical sexual abuse takes courage, especially if you’re feeling disconnected or weighed down by memories that seem impossible to quiet. It’s important to know that looking for support is not a weakness, it’s a brave act of self-care and the first step toward reclaiming your life. Healing from trauma is deeply personal, but you don’t have to navigate it alone; professional counseling offers a safe, steady space to understand what you’ve been through and begin to shape a gentler path forward.
What Is Trauma?
At its heart, trauma is the emotional response to a deeply distressing event that overwhelms your ability to cope. It’s not about the event itself, but how your mind and body react to it[1]. Think of it like a circuit breaker in a house. When there’s a sudden surge of electricity, the breaker trips to protect the system. Trauma is your nervous system’s way of tripping to protect you from an experience that’s just too much to process all at once. For survivors of physical or sexual abuse, this exposure can leave you feeling unsafe in your own skin long after the danger has passed. It’s important to remember that everyone’s response is unique. There's no right or wrong way to feel. If this experience is part of your story, you are not alone. Studies show that 60.7 percent of men and 51.2 percent of women report experiencing at least one trauma in their lifetime.
What Is PTSD?
Post-traumatic stress disorder, or PTSD, is a specific mental health condition that can develop after you’ve experienced or witnessed a traumatic event. It’s as if your brain gets stuck in high-alert mode, unable to file the memory away as "past." While many people experience short-term stress after trauma, PTSD symptoms persist and can interfere with daily life. These symptoms usually fall into a few key groups: intrusive memories like flashbacks or nightmares, avoiding reminders of the event, negative changes in your thoughts and mood, and feeling constantly on edge. It's a treatable condition, and understanding its criteria is often the first step toward a diagnosis and healing. In the U.S., about 3.5 percent of adults have PTSD in a given year, with women being more than twice as likely as men to develop the disorder. Seeking PTSD treatment is a common and courageous step for survivors of abuse.
What Is Complex Trauma?
Sometimes, trauma isn't a single event but a series of repeated or prolonged experiences, like ongoing childhood abuse, where there was no easy way to escape. This can lead to what's known as complex trauma, or C-PTSD. While it shares many features with PTSD, complex PTSD often comes with additional challenges. Survivors may struggle with emotional regulation, finding it hard to manage intense feelings. Relationships can feel difficult, especially with trust, and it can deeply affect your sense of self, leading to feelings of worthlessness or shame. If you find yourself struggling with these deeper patterns, know that it’s a completely understandable response to what you’ve been through.
Types of Trauma
Trauma can come from many different experiences, and while every story is valid, understanding the specific type of trauma you’ve faced can help you and your counselor find the most effective path to healing. Reading about these topics can be difficult, so please be gentle with yourself. The goal here is not to relive painful memories but to give a name to what you've experienced, which can be a powerful step in taking back control.
Adverse Childhood Experiences
Adverse Childhood Experiences, often called ACEs, are potentially traumatic events that occur in childhood (from birth to age 17). These can include experiencing physical, emotional, or sexual abuse, neglect, or witnessing violence in the home. It also includes household dysfunction, like a family member struggling with substance use or mental health issues. Research has shown that the more ACEs someone has, the higher their risk for various health problems in adulthood. For example, studies suggest that around 10 percent of children in the U.S. experience psychological abuse each year[2]. Healing often involves addressing the deep impact of this childhood trauma.
Sexual Assault/Rape
Sexual assault or rape is any type of sexual contact or behavior that occurs without explicit consent. It’s a profound violation of your safety and autonomy. If you are a survivor of sexual abuse, it is crucial to hear this: it was not your fault. The connection between sexual assault and PTSD is incredibly strong. In fact, for women, rape is the traumatic event most likely to cause PTSD, with one study finding a rate of 45.9 percent. Support is available to help you process what happened and navigate the complex feelings that follow.
Domestic Violence/Intimate Partner Violence
Intimate partner violence (IPV) isn't just a single fight; it's a pattern of abusive behaviors used by one person to maintain power and control over another in a relationship. This can include physical violence, sexual abuse, emotional manipulation, financial control, and stalking. It can happen to anyone, in any kind of relationship. Statistics show that between 2001 and 2005, IPV accounted for 21.5 percent of all nonfatal violence against women[3]. Understanding the dynamics of domestic violence is often the first step toward breaking the cycle.
Risk and Protective Factors
Why do some people develop lasting trauma while others seem to recover more quickly from similar events? The answer often lies in a combination of risk and protective factors. This isn’t about placing blame or judging anyone’s strength. It’s about understanding the complex web of experiences, biology, and support systems that shape our journey. Knowing these factors can help you recognize your own vulnerabilities and, more importantly, empower you to build up the supports that foster resilience.
Risk factors
Certain factors can make someone more vulnerable to the long-term effects of trauma. It's important to remember that having these risk factors doesn't mean a negative outcome is inevitable. They simply highlight areas where extra support might be needed.
- Individual Factors: Previous exposure to trauma, a family history of mental illness, or pre-existing mental health conditions can affect your ability to self-regulate thoughts and feelings after a new traumatic event.
- Relational Factors: A lack of strong, healthy social support from family or friends can leave you feeling isolated and alone in your struggle, making it harder to process what happened.
- Community and Societal Factors: Living in poverty, experiencing discrimination, or being exposed to neighborhood violence can create a constant state of stress that wears down your ability to cope with additional trauma.
Protective factors
Just as some factors increase risk, others can build resilience and help protect you from the lasting impact of trauma. The great thing about protective factors is that many of them can be learned and strengthened over time, especially with the right support.
- Strong Social Support: Having caring and supportive relationships with family, friends, or community members provides a critical buffer against stress[4].
- Positive Coping Skills: The ability to manage stress in healthy ways, such as through mindfulness, exercise, or creative outlets, can make a huge difference in your recovery.
- A Sense of Self-Efficacy: Believing in your own ability to handle challenges and influence your life's direction is a powerful tool for healing.
- Access to Resources: Having access to quality mental health care, safe housing, and community services provides a safety net that makes recovery possible[5]. Seeking professional help is one of the most important protective actions you can take.

Responses to Trauma: Trauma and Behavioral Health
Trauma doesn't just live in the past; it can ripple out and affect your overall mental and behavioral health in profound ways. When the nervous system is stuck in survival mode, it can lead to other challenges as you try to cope with the emotional pain. This often results in what are called co-occurring disorders, where trauma and another condition, like depression or a substance use disorder, exist at the same time. The good news is that integrated treatment, which addresses both the trauma and co-occurring disorders together, is highly effective.
Substance use disorders
There is a very strong link between trauma and substance use disorders. For many survivors, using alcohol or drugs can feel like a way to numb painful memories, quiet racing thoughts, or simply feel something different for a while. This is often called "self-medication." While it might offer temporary relief, it can create a cycle of dependence that complicates healing. Statistics show just how connected these issues are. For instance, women with alcohol dependence are 3.6 times more likely to have PTSD. In one study of people in outpatient substance abuse treatment, a staggering 88.6 percent reported experiencing at least one traumatic event[6].
Mood disorders
Trauma can significantly increase the risk for mood disorders, such as major depression or bipolar disorder. The persistent stress and negative alterations in thinking that come with trauma can disrupt the brain's chemistry, leading to symptoms like deep, lasting sadness, a loss of interest in things you once enjoyed, and difficulty regulating your emotions. Research confirms this connection, showing that individuals with PTSD are significantly more likely to also have major depression, dysthymia, or bipolar disorder compared to those without PTSD[7]. Addressing the root trauma is often key to finding lasting relief from these mood disorders.
Anxiety disorders
It makes sense that living through a terrifying experience can lead to ongoing anxiety. For trauma survivors, the world can feel like a dangerous place. The hypervigilance that helps you survive a threat can turn into generalized anxiety disorder (GAD), where you feel constant, excessive worry. It can also lead to panic disorder, characterized by sudden, intense panic attacks, or social anxiety. Among people with a past-year PTSD diagnosis, 35 percent reported having had one or more panic attacks. These anxiety disorders are your brain's attempt to protect you from future harm, but therapy can help teach it that the danger has passed.

Trauma-Specific Treatments
When you're ready to seek help, it's important to know that there are therapies designed specifically for healing from trauma. These aren't just about talking; they are evidence-based methods proven to help your brain and body process what happened. This work is often done within a framework of "trauma-informed care," which means your therapist understands the widespread impact of trauma and creates an environment that feels physically and emotionally safe[8]. Remember, there's no one-size-fits-all solution. Finding the right therapy and the right therapist is a personal journey, and a good counselor will work with you to find the best fit.
Cognitive–Behavioral Therapy
cognitive behavioral therapy, or CBT, is a type of talk therapy that helps you become aware of negative or inaccurate thinking so you can view challenging situations more clearly and respond to them in a more effective way. A specialized form called Trauma-Focused CBT (TF-CBT) is particularly effective for survivors of abuse, especially children and adolescents. It helps you process traumatic memories in a safe and structured way, manage difficult emotions, and develop healthy coping skills to move forward.
Eye Movement Desensitization and Reprocessing
eye movement desensitization and reprocessing (EMDR) is a powerful therapy that helps the brain reprocess traumatic memories that have gotten "stuck." During an EMDR session, you'll be asked to recall distressing events in brief doses while receiving bilateral sensory input, such as watching a light or listening to a tone from side to side. This process helps the brain resolve unprocessed traumatic memories, allowing you to remember the event without the intense emotional charge. EMDR is widely recognized as an effective, evidence-based treatment for PTSD[9].
Psychodynamic Approaches
psychodynamic therapy focuses on how your past experiences, particularly those from early childhood, unconsciously shape your current feelings and behaviors. In the context of trauma, this approach helps you explore the deep-seated impact of the abuse on your sense of self, your patterns in relationships, and your core beliefs. By bringing these unconscious dynamics to the surface, you can gain powerful insight and self-awareness, which is the foundation for lasting change and healing.
GENERAL GUIDELINES FOR TREATMENT
Taking the step to find a therapist is one of the most empowering things you can do for yourself. The connection you have with your counselor is one of the most important parts of the healing process, so it's worth taking the time to find someone who feels like a good fit. You are in control of this journey.
- Look for a trauma specialist: Seek out counselors who specialize in trauma, PTSD, or the specific type of abuse you experienced. They will have the training and understanding needed to support you safely. The SAMHSA National Treatment Locator can be a helpful starting point.
- Ask questions: Don't be afraid to ask a potential therapist about their approach. You can ask what types of therapy they use (like EMDR or TF-CBT), what their experience is with survivors of abuse, and what a typical session looks like. Another valuable resource is the Indiana DMHA Treatment Finder.
- Trust your gut: Do you feel heard, respected, and safe with this person? Therapy is a vulnerable process, and it’s essential that you feel comfortable with the person guiding you. It's perfectly okay to speak with a few different counselors before you decide.
- Discuss logistics: Before you start, make sure you understand their fees, whether they accept your insurance, and their cancellation policy. This helps avoid any stress down the road.
Remember, healing is not a straight line. It’s a personal journey with its own pace and rhythm. Taking the first step to find help is a testament to your strength and resilience. You have already survived so much, and you deserve a future where you feel safe, whole, and at peace. If you're ready to talk, our compassionate team at Indiana Rehabs is here to listen without judgment and help you find the right path forward. You can call us anytime at (888) 568-9930 or get in touch through our contact page. You don’t have to do this alone.
Frequently Asked Questions About Counseling for Physical and Sexual Abuse
How do I know if I need counseling for physical or sexual abuse?
What happens during the first counseling session for trauma?
How long does counseling for sexual abuse last?
Can counseling help if the abuse happened a long time ago?
Will I have to talk about the details of the abuse in therapy?
Is everything I say in therapy confidential?
- Substance Abuse and Mental Health Services Administration. (11-08-2024). Trauma and violence. Substance Abuse and Mental Health Services Administration. samhsa.gov
- (2024-10-24). Trauma-informed health care. County Health Rankings & Roadmaps. countyhealthrankings.org
- Substance Abuse and Mental Health Services Administration. (09-09-2025). Key resources and tools for NSDUH, CBHSQ data. Substance Abuse and Mental Health Services Administration. samhsa.gov
- Mental Health America of Indiana. (2021). Mental Health America of Indiana strategic plan 2021 - 2025. Mental Health America of Indiana. mhai.net
- U.S. Department of Health & Human Services. (n.d.). State residential treatment for behavioral health conditions: Indiana. U.S. Department of Health & Human Services. aspe.hhs.gov
- Indiana Division of Mental Health and Addiction. (n.d.). Drug fact sheet: Substance use in Indiana, SFY 2024. Indiana Division of Mental Health and Addiction. in.gov
- (2008-05-01). Prevalence and treatment of depression and posttraumatic stress disorder in a primary care clinic. Journal of the National Medical Association. pmc.ncbi.nlm.nih.gov
- Indiana University School of Medicine. (02-07-2021). Opioids abuse crisis. Indiana University School of Medicine. medicine.iu.edu
- Substance Abuse and Mental Health Services Administration. (01-08-2025). Evidence-based practices resource center. Substance Abuse and Mental Health Services Administration. samhsa.gov
