Rehabs for Chronic Pain

Showing 20 of 45 Results (filtered)
Featured Rehab Centers

1525 West Harrison street, Plymouth, IN 46563

91 West Mound Street, Nashville, IN 47448



Addiction Rehab Centers - ARC At Bayside | Indianapolis Drug & Alcohol Rehab
Indianapolis, Indiana
5929 Lakeside Blvd, Indianapolis, IN 46278
Get Personalized Rehab Matches in 60 Seconds
Tell us a few details and we’ll show a personalized shortlist of verified Indiana rehabs, making it simple to compare options and choose your next step with confidence.



Alliance MD - Addiction Treatment Center
Merrillville, Indiana
8102 Georgia St, Merrillville, IN 46410

Hamilton Center Inc: Mathew Maleakal S MD
Terre Haute, Indiana
620 8th Ave, Terre Haute, IN 47804



IU Health Addiction Treatment & Recovery Center
Indianapolis, Indiana
1701 N Senate Ave STE C-3, Indianapolis, IN 46202


Methodist Hospitals Rehab Center
Merrillville, Indiana
101 E 87th Avenue Pavilion A, Third Floor, Merrillville, IN 46410



NorthShore Health Frontline Foundations
Chesterton, Indiana
801 Broadway Ave, Chesterton, IN 46304


Samaritan Center - Vincennes
Vincennes, Indiana
121 Buntin Street, Vincennes, IN 47591



Boca Recovery Center - Fort Wayne, Indiana
Fort Wayne, Indiana
111 W Berry St #211, Fort Wayne, IN 46802
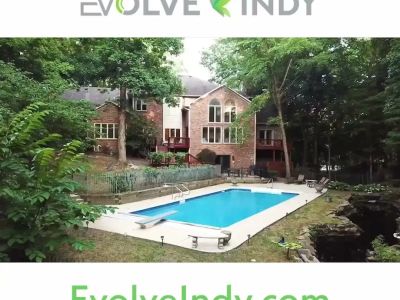


Evolve Indy
Indianapolis, Indiana
8770 Guion Rd, Indianapolis, IN, 46268



Dr. Malek’s Office – Primary Care, Senior Care & Mental Health
Evansville, Indiana
4972 Lincoln Ave #101, Evansville, IN 47715



CleanSlate Outpatient Addiction Medicine
Greencastle, Indiana
833 Indianapolis Rd Suite E, Greencastle, IN 46135



CleanSlate Outpatient Addiction Medicine Merrillville
Merrillville, Indiana
8601 Connecticut St, Merrillville, IN 46410



Indiana Center for Recovery
Bloomington, Indiana
1004 West 1st Street, Bloomington, IN, 47403



CleanSlate Outpatient Addiction Medicine
Muncie, Indiana
124 E Main St, Muncie, IN 47305



Kentuckiana Integrative Medicine
Jeffersonville, Indiana
405 E Court Ave #102, Jeffersonville, IN 47130



First City Recovery Center
Kokomo, Indiana
317 W Jefferson St, Kokomo, IN, 46901



Lafayette Regional Rehabilitation Hospital
Lafayette, Indiana
950 Park E Blvd, Lafayette, IN 47905


Why Trust Indiana Rehabs
As Hoosiers helping Hoosiers, we understand the unique challenges our communities face. Our team meticulously verifies every Indiana treatment center, ensuring you find trusted, local care that truly understands your journey.
About our listingsLevels of Care
Explore popular treatment options by levels of care, from flexible treatment in Outpatient centers to intensive care in Residential rehabs.
Free · 24/7 · Confidential
Talk to a Treatment Specialist
Call now to get matched with Indiana facilities that accept your insurance.
(888) 568-9930
Free
Ins. check
4.9★
Rating
HIPAA
Protected
Can't travel to a facility?
Licensed Indiana therapists via secure video — same-week appointments, evenings & weekends available.
More than one in five adults in the U.S. live each day with chronic pain—so if it feels like you’re carrying an invisible weight, you’re far from alone. But pain doesn’t have to rule your story or become a permanent cloud over your days. With the right mix of medical support, practical strategies, and gentle changes in daily habits, it’s possible to carve out real space for comfort, movement, and hope again.
What is chronic pain?
Think of acute pain as your body’s alarm system. When you sprain an ankle or touch a hot stove, that sharp, immediate pain is your body telling you something is wrong. It’s a direct response to an injury, and it usually goes away once you’ve healed. Chronic pain, on the other hand, is like an alarm that keeps ringing long after the danger has passed. It’s defined as persistent pain that lasts for more than three to six months, continuing even when the original injury or illness has healed.
It’s a reality for millions of people. In fact, about 20.9% of adults in the U.S. live with chronic pain, which shows just how many lives are touched by this condition[1]. For many patients, this happens because the nervous system itself can change. Over time, it can become overly sensitive and reactive, a process known as central sensitization. This means your brain and nerves start to interpret normal signals, like light touch, as painful. It’s not "all in your head"; it’s a real, physical change in how your body processes pain. Understanding this is the first step toward managing it, because it shifts the focus from just treating a symptom to caring for your overall health and well-being.
What causes chronic pain?
Chronic pain can feel like a mystery, and sometimes, its exact cause is hard to pin down. It might start with a clear event, like a car accident or a surgery, but in other cases, it can develop without any obvious injury at all. Your emotional well-being also plays a role; feelings of stress, anxiety, or depression can actually make pain feel more intense. It’s a complex mix of physical and emotional factors that are unique to each person.
Several conditions are well-known for causing chronic pain, including:
- Arthritis: Joint inflammation and pain, often in the hands, knees, or hips.
- Fibromyalgia: Widespread muscle pain accompanied by fatigue, sleep, and memory issues.
- Migraines and Headaches: Severe, recurring headaches that can be debilitating.
- Nerve Damage (Neuropathy): Often described as a shooting, burning, or tingling pain.
- Back Problems: Issues like herniated discs or spinal stenosis are common culprits.
Certain risk factors can also increase the chances of developing chronic pain. These include getting older, having a previous injury, genetics, and carrying extra weight, which puts more stress on your joints[2]. While you can’t change things like age or genetics, knowing these risk factors helps you and your doctor create a plan that supports your whole health, not just the pain itself.
Symptoms and How Chronic Pain is Diagnosed
If you were to ask someone what chronic pain feels like, you’d get many different answers. It’s not just one sensation. For some, it’s a dull, constant ache. For others, it’s a sharp, shooting, or burning feeling. It might throb, sting, or feel like an electric shock. This pain can significantly impact your quality of life, making it hard to do the things you once enjoyed.
Beyond the pain itself, it often brings along other unwelcome symptoms. It’s common for people to experience:
- Constant fatigue or feeling drained
- Trouble with sleep, either falling asleep or staying asleep
- A decreased appetite
- Irritability, anxiety, or mood swings
- Symptoms of depression, like feeling hopeless or losing interest in activities

Getting a diagnosis starts with a conversation. Your healthcare provider will want to know your full medical history and listen carefully as you describe your symptoms. They’ll likely perform a physical exam to check your range of motion and reflexes. In some cases, they may order imaging tests like X-rays or an MRI to look for injuries or rule out other conditions. Nerve studies can also help pinpoint the source of the pain. The most important part of this process is being open and honest. The more details you can share about what you’re feeling, the better your healthcare provider can help you find answers and create a path forward.
What is the treatment for chronic pain?
When it comes to chronic pain management, there’s no one-size-fits-all solution. The most effective approach is a comprehensive one that’s tailored just for you, combining different therapies to address the physical, emotional, and psychological sides of pain. It’s helpful to know that for many treatments, the goal isn't always to eliminate pain completely. Instead, many modern approaches aim for about a 30% reduction in pain, which can be enough to dramatically improve your ability to function and enjoy life again. A multidisciplinary pain rehabilitation program often brings together medical, physical, and psychological therapies to give you the best chance at lasting relief[3].
Medical and Interventional Treatments
Your doctor might start with medications or procedures designed to reduce your pain signals. These can include:
- Over-the-counter (OTC) medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can help with pain caused by inflammation.
- Prescription medications: Your doctor might prescribe non-opioid medications first. Certain antidepressants can help with nerve pain, as can some anti-seizure drugs.
- Opioids: These powerful pain relievers are typically reserved for severe cases or short-term use after surgery. Due to the high risk of dependence and side effects, they are used with extreme caution for chronic pain.
- Injections and nerve blocks: Steroid injections can reduce inflammation in specific areas, while nerve blocks can interrupt pain signals before they reach the brain.
- Acupuncture: This traditional therapy involves inserting thin needles into the skin to stimulate specific points on the body and can be effective for some types of pain.
Physical Therapy and Lifestyle Therapies
Moving your body can be one of the best things you do for chronic pain, as long as it’s done safely. A physical therapist is an expert in creating exercise programs that are designed for you. They can help you improve your strength, flexibility, and posture without making your pain worse. Occupational therapy is another great resource; it helps you find new ways to do daily tasks that may have become difficult. Other helpful therapies include massage to soothe sore muscles and heat or cold therapy to reduce inflammation. Gentle, regular exercise like walking, swimming, or yoga can release endorphins, your body’s natural pain relievers, and improve your overall well-being.

Cognitive–Behavioral Therapy
Pain isn't just a physical sensation; it has a powerful emotional component, too. Cognitive behavioral therapy (CBT) is a type of talk therapy that helps you recognize and change the negative thoughts and behaviors that can make pain worse. It’s not about convincing you the pain isn’t real. Instead, CBT gives you practical coping skills to manage how you respond to pain. You learn to challenge thoughts like, “This pain will never end,” and replace them with more balanced ones. This process can help you feel more in control. Other psychological supports, like mindfulness meditation and biofeedback, can also provide you with tools to calm your nervous system and reduce the stress that often comes with chronic pain.
The Link Between Chronic Pain and Mental Health
Living with constant pain is exhausting, and it’s completely understandable that it can take a toll on your mental health. The daily struggle can lead to feelings of frustration, sadness, and isolation, which are classic signs of depression and anxiety. It works the other way, too. If you’re already dealing with depression, it can actually make your pain feel worse. Your brain and nervous system are wired in a way that makes pain and emotions deeply connected. This can create a difficult cycle: pain worsens your mood, and a low mood amplifies your pain.
You’re not alone in this experience. It's estimated that a significant number of people with chronic pain also have a co-occurring mental health condition like depression[4]. That’s why the most effective chronic pain management plans always include support for your mental and emotional well-being. Addressing your psychological health isn’t just an add-on; it’s a core part of feeling better physically. When you treat both the body and the mind, you have a much better chance of breaking the cycle and improving your overall quality of life.
Navigating Chronic Pain and Substance Use
The relationship between chronic pain and substance use is incredibly complex, especially when it comes to prescription opioids. For decades, opioids were seen as a primary solution for severe pain, but we now understand the serious risks that come with them, particularly when used long-term[5]. When you take an opioid medication regularly, your body can build up a tolerance, meaning you need more of it to get the same relief. This can lead to physical dependence, where your body needs the drug to function normally, and can sometimes escalate to an addiction[6].
For individuals with a history of substance use disorder, managing chronic pain requires an even more careful and thoughtful approach. The focus is almost always on non-opioid treatments to avoid triggering a relapse and to protect their recovery. This is where integrated care becomes so important. A treatment plan that involves both pain specialists and addiction professionals ensures that every aspect of a patient’s health is considered. By working together, they can create a safe, effective strategy that manages pain without compromising the hard work of recovery. It’s about finding a path to relief that supports long-term health and well-being in every sense.
Living Well with Chronic Pain: Daily Management Tips
Managing chronic pain is an ongoing process, but there are small, practical things you can do every day to feel more in control and improve your quality of life. These strategies focus on creating balance and building resilience.
- Practice Activity Pacing: This is about finding the sweet spot between doing too much and too little. Instead of pushing through until you’re exhausted, break up tasks into smaller chunks and take planned rest breaks. It helps you stay active without causing a pain flare-up.
- Focus on Stress Management: Stress is a major trigger for pain. Simple techniques like deep breathing, listening to calming music, or spending time on a hobby you love can help calm your nervous system[7].
- Improve Your Sleep Hygiene: Pain can disrupt sleep, and poor sleep can worsen pain. Try to go to bed and wake up around the same time every day, create a relaxing bedtime routine, and make sure your bedroom is dark, quiet, and cool.
- Eat a Healthy Diet: Some foods can increase inflammation, while others can help reduce it. Focusing on anti-inflammatory foods like leafy greens, berries, fish, and nuts can support your body’s overall health.
- Find a Support Group: Connecting with others who understand what you’re going through can make a world of difference. Whether it’s in person or online, a support group can be a source of encouragement and practical advice.

Remember to be gentle with yourself. Living well with chronic pain is about progress, not perfection. Every small step you take is a victory.
Find Hope and Professional Support in Indiana
The journey of chronic pain management is an active one, but you don't have to walk it alone. With the right team and a personalized plan, it is possible to reduce your pain and reclaim parts of your life that you thought were lost. If your pain is persistent, getting worse, or making it hard to get through your day, it's time to seek professional support. A healthcare provider can help you find the source of your pain and guide you toward effective treatments.
When you meet with a provider, it can be helpful to have some questions ready. You might ask:
- What are my non-opioid treatment options?
- How can we incorporate mental health support into my plan?
- What kind of physical therapy or exercise would be safe for me?
Finding the right team is a critical step in your recovery. You can use a trusted resource like the SAMHSA National Treatment Facility Locator to find licensed providers near you. Taking that first step to ask for help is an act of strength and hope.
Managing chronic pain is a journey, not a destination, but you don't have to face it by yourself. With a combination of medical treatments, lifestyle adjustments, and strong emotional support, you can find relief and improve your quality of life. If you're ready to explore your options and find a team that understands, help is available right here in Indiana. Please don't hesitate to call us at (888) 568-9930 to learn more about our programs. At Indiana Rehabs, we're here to help you connect with the support you need. You can also get in touch through our contact page to start the conversation.
- Centers for Medicare & Medicaid Services. (09-26-2024). Graham pain management study. CMS.gov. cms.gov
- Trust for America's Health. (05-24-2023). Pain in the Nation: The drug, alcohol and suicide crises. Trust for America's Health. tfah.org
- (04-10-2025). Patient and health service factors associated with enrollment in a multidisciplinary pain rehabilitation program. IUPUI ScholarWorks. scholarworks.indianapolis.iu.edu
- Indiana Division of Mental Health and Addiction. (2024). Drug Fact Sheet: Substance Use in Indiana, SFY 2024. Indiana Family and Social Services Administration. in.gov
- Indiana University School of Medicine. (02-07-2021). Opioids abuse crisis. Indiana University School of Medicine. medicine.iu.edu
- Reisner, M. D., et al. (2019). Long-term prescription opioid utilization, substance use disorders, and overdose. Journal of General Internal Medicine. pmc.ncbi.nlm.nih.gov
- Substance Abuse and Mental Health Services Administration. (11-08-2024). Trauma and violence. SAMHSA. samhsa.gov
